In October, Democratic Gov. Andy Beshear announced the expansion of dental, vision and hearing benefits for 900,000 Kentucky adults on Medicaid. On March 16, 2023, the Republican-controlled General Assembly took a final vote to take those benefits away, calling the regulation used to install them deficient. Beshear said Thursday that he will find a way to keep them in place.
In presenting Senate Bill 65, Sen. Stephen West (R-Paris) said the regulation Beshear issued to expand these services was deficient because the funding came from the $38 million in savings that came when the state moved to a single pharmacy benefit manager, a middleman between drug manufacturers and companies that manage Medicaid.
West said using these savings amounted to the governor “appropriating money” and that lawmakers should have been involved in how it was spent.
“It was a huge change, really that should have been done through, we felt, through statute through involving the legislature,” West said at the Feb. 15 Senate State and Local Government Committee meeting.
In October, Cabinet for Health and Family Services spokeswoman Susan Dunlap told the Courier Journal that federal funds would cover 90% of the expansion’s cost. She said the state’s move to one pharmacy-benefits manager last year “has resulted in significant ongoing savings to the Medicaid program that will provide enough funding for this program moving forward.”
As SB 65 went through the legislature, it was amended to extend dental, vision, and hearing services through June 30 to allow people already getting the services to receive them and allow providers to be paid.
The amendment also says nothing in the bill should be construed to prohibit the state Medicaid department from increasing reimbursement rates, long a goal of health-care providers. The Kentucky Oral Health Coalition says Medicaid's dental provider rates have been stagnant for more than 20 years.
Sen. Stephen Meredith (R-Leitchfield) said a rate hike is especially needed in medically disadvantaged areas. In explaining his vote for SB 65, he also said the money could have been used to help the 5,000 children who are waiting for services from one of the state’s special Medicaid waiver programs.
“I just want to remind folks that what we’re asking here is for some involvement from the legislature,” Meredith said. “Talk to us. Let us have some input in this.”
What’s next?
Before the expansion of these services, they were offered on a limited basis.
Dental services for adults were limited to an annual cleaning and extractions linked to certain medical conditions. Adult fillings were not covered. The expansion allowed coverage for fillings, dentures, implants, root canals, extractions, restorations, periodontics and an additional cleaning each year.
Also, under the old rules, a Medicaid enrollee could be evaluated for hearing loss only on referral from their primary-care doctor; and glasses and contact lenses were not covered, though exams were. Some managed-care firms offered some of these services as an incentive to get people to enroll with them.
Asked at his weekly news conference Thursday if there is a way to maintain the benefits, Beshear said, “I believe a new regulation will allow for the continuation of vision, dental and hearing benefits. The expansion of those benefits, the funding coming from the federal government is an executive branch function. But even at the hearing, I believe ... one of the legislators said it looks like you’ll need a new regulation.”
SB 65 requires any new regulation to be substantially different from the original. If Beshear vetoes the bill, the legislature could easily override the veto.
Beshear called the need for dental, vision and hearing benefits for people on Medicaid a “no-brainer” because “This is what gets people back to work.” He elaborated:
“There's a study that talks about over 100 million work hours lost due to dental, emergency dental procedures that if you have coverage you avoid. Now there are studies out there about the number of people that can’t go to work because we don’t cover getting them a pair of glasses. And then think about safety on the job site. You know a ton of Americans ... suffer from hearing loss. And to be able to get to the job and to do it correctly, you need to have that type of coverage. Again, if we care about the workforce, right, let’s take the basic steps to get more people healthy [and] back to work.”
Access to providers
West also argued that health-care providers tell lawmakers that even if these services are permitted in Medicaid, the program’s reimbursements are so low that it will be hard for the patients to find providers.
That said, the health cabinet says thousands of Kentuckians on Medicaid have already taken advantage of these services since they became available Jan. 1.
“As of Feb. 22, more than 8,000 Kentuckians — across all 120 counties — have already received dental, vision, and hearing services they need under these regulations,” the cabinet said. “More than 1,000 Kentuckians received nearly 3,330 dental services under these regulations — in all 120 Kentucky counties — including from a dentist in Clay County who since Jan. 1, 2023, had provided four sets of dentures for patients and has 44 more sets of dentures in progress.”
Clay County is the home of Senate President Robert Stivers (R-Manchester).
The cabinet added, “Nearly 7,000 Kentuckians have received vision services under these regulations, with nearly 43,000 services provided. And 40 Kentuckians have received hearing services with these regulations in place. ... Providers have received over $1 million in reimbursement for the services.”
Health advocates push back
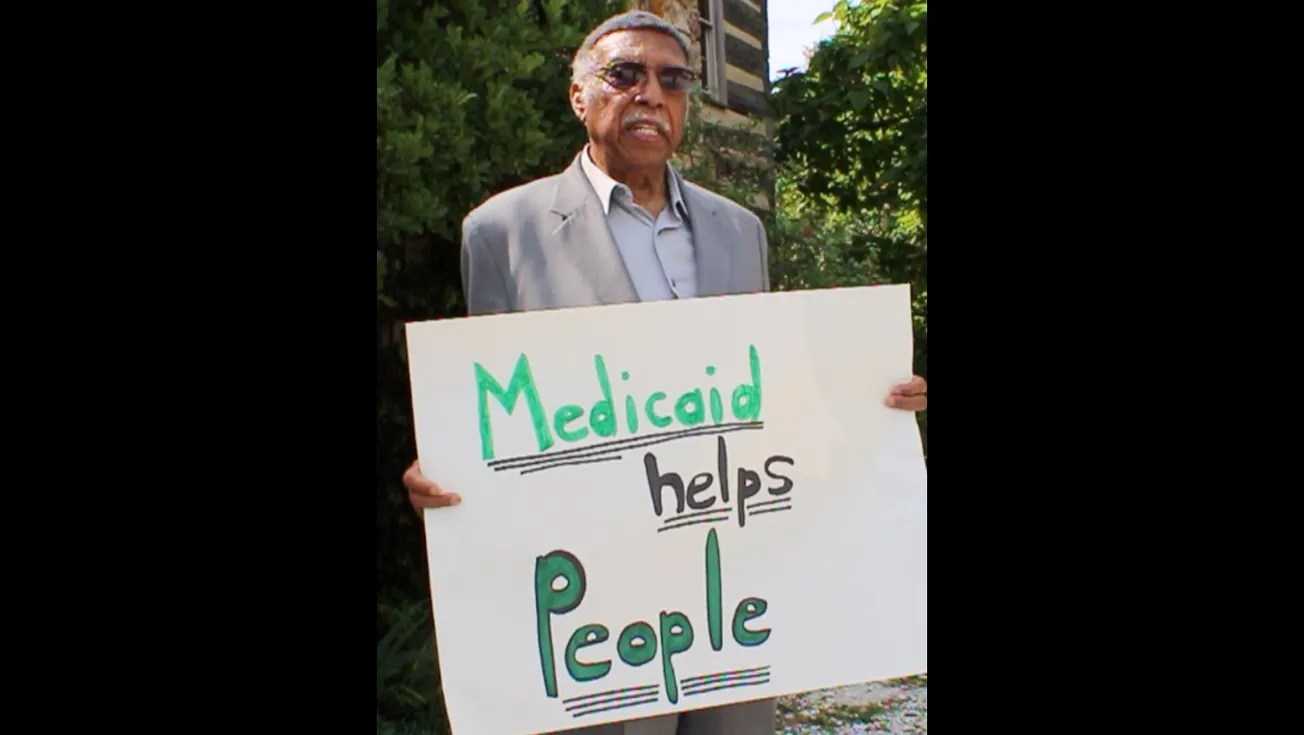
Health advocates were disappointed in the bill’s passage and called for legislators to reinstate thes services.
“The genesis of this unfortunate piece of legislation is a raw partisan battle between the General Assembly and the governor,” said Terry Brooks, executive director of Kentucky Youth Advocates. “Both branches of our government should be holding each other accountable when one thinks the other overstepped its bounds. Yet, there should also be no doubt that neither providers nor Kentucky families should pay the price for a political food fight. SB 65 has providers left holding the bag with more Kentuckians losing dental benefits than the total population of Alaska. It’s as unwise as it is unfair.”
In a statement about the passage of SB 65, the Oral Health Coalition cited the great need for comprehensive dental services in Kentucky, noting that the state ranks among the bottom five states on several oral-health indicators and has more seniors with no natural teeth than any other state.
“While it was a worthy debate about the process to expand services, the reality now is that 900,000 low-income, disabled, and other vulnerable Kentucky adults must once again go without critical dental care,” the coalition said. “By no means is this expansion the answer to the growing oral health crisis in Kentucky, but it can offer a first step toward providing comprehensive dental care for Kentuckians. The Department for Medicaid Services and the General Assembly must reach an agreement in the immediate aftermath of the legislative session so our Commonwealth can be back on track to providing folks with the health care they need to be healthy, work, and thrive.”
Emily Beauregard, executive director of Kentucky Voices for Health, an advocacy group, told Kentucky Health News in an e-mail, “Regardless of the politics, it’s clear that Kentuckians don’t have enough access to the dental, vision, and hearing care they need to be healthy. We’ve made progress in recognizing that mental health is health and we need to do the same for our mouths, eyes, and ears.”
She added, “Whether it’s through regulation or legislation, we need policymakers to increase access to these services to improve population health and build a stronger workforce,” she added. With the passage of SB 65, “I hope legislators will take action to increase services through legislation instead.”
--30--
Written by Melissa Patrick. Cross-posted from Kentucky Health News.